Very Preterm Births
Summary Indicator Report Data View Options
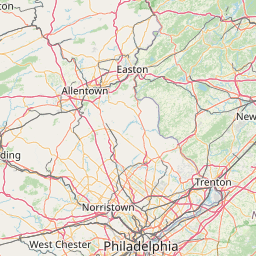
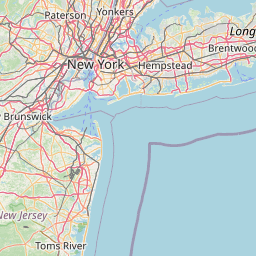
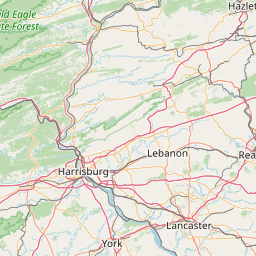
Very Preterm Births by County of Residence among Singletons, New Jersey, 2018-2022

Why Is This Important?
Prematurity increases the risk for infant morbidity and mortality. Infants born preterm are at greater risk of dying in the first month of life. Preterm infants may require intensive care at birth and are at higher risk of developmental disabilities and chronic illnesses throughout life. They are more likely to require special education services. Health care costs and length of hospital stay are higher for preterm infants. The more preterm an infant is born, the more severe the health problems are likely to be.
Definition
Percent of live births before 32 weeks of gestation based on obstetric estimate
Preterm is synonymous with premature. Infants born before 37 weeks of pregnancy are considered preterm and those born before 32 weeks of pregnancy are considered very preterm. Infants born at or after 37 weeks of pregnancy are called full term. Most pregnancies last around 40 weeks.
Data Sources
- Birth Certificate Database, Office of Vital Statistics and Registry, New Jersey Department of Health
(https://www.nj.gov/health/vital/) - Natality public-use data, CDC WONDER On-line Database, Centers for Disease Control and Prevention
(https://wonder.cdc.gov/natality.html)
How the Measure is Calculated
| Numerator: | Number of live births before 32 weeks of gestation based on obstetric estimate |
| Denominator: | Total number of live births |
How Are We Doing?
New Jersey's overall very preterm birth rate decreased from its peak of 1.8% in 2006 to 1.3% in 2020-2022 and, among singletons, the rate declined from 1.4% in 2000 to 1.1% in 2019-2022. Very preterm birth is highly correlated with plurality. While 1.1% of singletons were born very preterm, 8.2% of twins, and more than one-quarter of triplet and higher order births were born prior to 32 completed weeks of gestation in 2022. Among singletons, very preterm rates were lowest in Hunterdon County (0.6%) and highest in Essex and Cumberland Counties (1.7%) in 2018-2022.
What Is Being Done?
The Division of Family Health Services in the New Jersey Department of Health administers programs to enhance the health, safety and well-being of families and communities in New Jersey. Several programs are aimed at improving birth outcomes.
Evidence-based Practices
CDC Grand Rounds: Public Health Strategies to Prevent Preterm Birth
More Resources
Preterm Birth: https://www.cdc.gov/maternal-infant-health/preterm-birth/index.html
National Center for Health Statistics Birthweight and Gestation Fast Stats: https://www.cdc.gov/nchs/fastats/birthweight.htm
Health Program Information
The New Jersey Department of Health has been using the obstetric estimate (OE) to determine gestational age since 1989, while the National Center for Health Statistics (NCHS) had been calculating it using date of last menstrual period (LMP). In 2003, NCHS changed the standard for gestational period from the LMP-based gestational age to the OE-based gestational age. OE-based gestational age for U.S. data became available for years 2007 and later in February, 2016. Data in reports published prior to February, 2016 will not match data shown here. Refer to Measuring Gestational Age in Vital Statistics Data: Transitioning to the Obstetric Estimate for more information.
The annual number of birth records with unknown gestational age was between 5,100 and 6,700 in 2000-2009. Unknown gestational age dropped to 1,000-2,800 records per year in 2010-2014. In recent years, improved data exchange between states has resulted in fewer than 100 NJ resident birth records with unknown gestational age most years. A large number of "unknowns" in the denominator may artificially decrease rates.
 Official Site of The State of New Jersey
Official Site of The State of New Jersey
